-
 Triluma 15 gm CreamUS$ 23.83 - US$ 33.00
Triluma 15 gm CreamUS$ 23.83 - US$ 33.00$23.83 - $33.00
Generic For : TrilumaActive Ingredient : Hydroquinon 4%, Tretinoin 0.05%, Fluocinolone 0.01% Topical Cream1 CreamUS$ 33.00 -
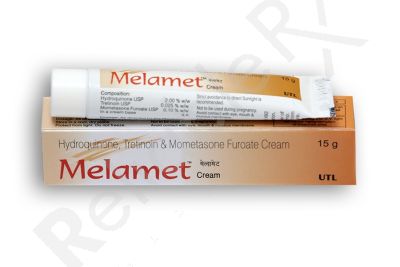 MelametUS$ 9.00 - US$ 11.00
MelametUS$ 9.00 - US$ 11.00$9.00 - $11.00
Generic For : Skin LiteActive Ingredient : Hydroquinone 2%, Tretinoin 0.025%, Mometasone Furoate 0.1%1 Tube/sUS$ 11.00
Melasma is a slowly developing hyperpigmentation disorder. It is also called chloasma, or the mask of pregnancy, and results in the most symmetrical brown pigmentation affecting the face and, occasionally, the forearms and back. The global prevalence of melasma is about 1%, although higher rates have been reported among individuals with darker skin types. Women are more likely than men to develop melasma, with an average age of onset between 20 and 50 years. However, the hyperpigmentation disorder can begin in adolescence and is thought to occur because of the hormonal factors. The condition frequently involves the face and poses a therapeutic challenge.
Understanding melasma
Melasma is a chronic pigmentary skin disorder that causes brown, grey-brown, or dark patches on sun-exposed areas of the face. It is more common in women than men, and it affects people between the ages of 20 and 50. It is also known as the "mask of pregnancy" when it emerges during pregnancy due to hormonal changes. Melasma does not cause any physical harm, but it can have significant social and psychological impacts. The visible brown patches on the face cause distress, impacting self-confidence and quality of life. It isn't easy to treat and has a high recurrence rate; understanding the condition in depth is important for effective treatment and management.
Melasma involves overactivity of melanocytes (the cells that produce melanin, the pigment that gives skin its colour), leading to hyperpigmentation. During melasma, these cells overproduce melanin, which deposits in the skin, leading to visible dark patches.
Typical location of lesions: Melasma typically presents as symmetric patches on the cheeks, forehead, nose bridge, and chin. It can also affect the neck, forearms, and other areas exposed to ultraviolet (UV) light.
Causes and risk factors of melasma
Genetic, hormonal, and environmental factors contribute to the development of melasma. While the exact cause of melasma is not fully understood, several risk factors have been identified.
- Sun exposure - Ultraviolet rays from the sun are the most significant cause of melasma. Sunlight stimulates melanocytes to increase melanin production, darkening pigmentation and worsening melasma.
- Hormonal influences - Hormone alternation plays a central role in melasma development:
‒ Pregnancy (particularly in the second and third trimesters)
‒ Oral contraceptives
‒ Hormone replacement therapy. Estrogen and progesterone appear to activate melanocyte activity, although the exact mechanisms are complex.
- Genetic predisposition - Individuals with a family history of melasma are more likely to develop it. The condition is also more common in:
‒ People with darker skin tones
‒ Individuals of Hispanic, Asian, Middle Eastern, or African descent.
- Medications and cosmetics - Some medications and skincare products can accelerate or trigger melasma by making the skin more sensitive to sunlight or by irritating it.
Diagnosis of melasma
Diagnosing involves the following methods:
- Clinical examination - A dermatologist evaluates the distribution and appearance of skin pigmentation.
- Wood's lamp examination - A special ultraviolet machine helps in determining the depth of pigmentation in the skin:
‒ Epidermal melasma - pigment in the upper layers of the face (easy to treat)
‒ Dermal melasma - pigment deeper in the skin (resistant to treatment)
‒ Mixed type - characteristics of both- This classification helps in deciding the treatment methods.
Management of melasma
Management of melasma requires a professional approach by your dermatologist. Be sure to receive the best care possible.
General treatment guidelines
Numerous treatments have been developed to address melasma, but there is no cure. While the appearance of melasma reduces after pregnancy or discontinuing a contraceptive pill, it may stay on your skin for many years or can stay for a lifetime.
- Sun protection
A major part of melasma management. Without sun protection, the best treatment methods won't help. Important things to do to protect skin from the sun are:
‒ Use broad-spectrum sunscreen (SPF 30 or higher) daily
‒ Wearing wide-brimmed hats and sunglasses
‒ Avoiding sun exposure during peak UV hours (10 a.m.- 4 p.m.)
‒ During outdoor activities, reapply sunscreen every two hours.
- Topical treatment
The first line of treatment is topical depigmenting agents, including hydroquinone, retinoids, azelaic acid, kojic acid, and combination cream (e.g., Tri-Luma)
- Procedural treatments
These treatments are used when topical treatments are not sufficient; they include chemical peels, microdermabrasion, and laser and light therapies (with caution, as they may worsen pigmentation).
- Oral agents
In select cases, oral medication like tranexamic acid may be prescribed under medical supervision.
If you are diagnosed with melasma, stop using skin care products, including facial cleansers, soaps, creams, or makeup, that cause skin irritation immediately. If the reason behind your melasma is your contraceptive pill, immediately stop taking it or change it to a lower estrogen dose. One can also use Tri-Luma 15 mg to treat melasma. The topical preparation provides quicker, more productive results than bleaching creams available on the market. It contains Hydroquinone, tretinoin, and Fluocinolone. Hydroquinone is one bleaching agent that works really well for melasma.
Hydroquinone: The best and most effective solution for melasma
Hydroquinone is considered one of the best and most effective treatment options for melasma patches on the skin. The creams do not bleach the skin; instead, they reduce the activity of pigment-producing cells. The condition generally improves within 3 to 4 months when used regularly. The improvement will begin to be seen in as little as 2 to 4 weeks.
Hydroquinone is one of the most commonly prescribed and studied agents for the treatment and management of melasma. It is classified as a first-line therapy in many clinical settings.
Working mechanism of the melasma cream
It works by inhibiting tyrosinase, an enzyme which regulates melanin production. Blocking the enzyme prevents the conversion of the amino acid tyrosine into melanin. As melanin production decreases, the existing pigment gradually fades. Hydroquinone is generally formulated at 2% (over-the-counter) or 4% (prescription). A higher concentration is advised for use under medical supervision.
Treating melasma with hydroquinone
Hydroquinone reduces existing pigmentation, prevents further melanin deposition, and works best when combined with sun protection and other therapies.
Results are seen within 8-12 weeks, but continued use for longer durations may be necessary for sustained improvement.
Who should not use hydroquinone?
A few precautions should be followed while using the medication:
‒ Avoid using during pregnancy or breastfeeding
‒ People with known sensitivity should not use the medicine
‒ People with eczema, dermatitis, or very sensitive skin should not use it
Side effects of hydroquinone
There are some common side effects of the medicines:
‒ Redness and irritation
‒ Dryness and peeling
‒ Burning or stinging sensation
‒ Contact dermatitis
Long-term or inappropriate use may lead to a rare, severe condition called exogenous ochronosis (bluish-black skin discolouration), which is very difficult to treat.
Warnings for hydroquinone
To minimise the side effects, keep the following things in mind:
‒ Use it under the supervision of your dermatologist
‒ Use it on the affected areas only
‒ Don't use it on broken or irritated skin
‒ always use it along with the sunscreen
Tri-Luma cream: Why is it effective for melasma?
Tri-Luma cream, containing tretinoin, hydroquinone, and fluocinolone, is specifically formulated to enhance the depigmenting effect. It has been found to be extremely effective in reducing the appearance of stubborn brown and grey patches. It is always better to talk to a dermatologist before purchasing any prescription topical medicine, such as Tri-Luma 15 mg. After you receive the prescription, follow your dermatologist's directions carefully to get the maximum benefit from this triple-combination medicinal cream. Using it appropriately will help you avoid irritation and adverse reactions. A high-quality sunscreen with a high SPF should be applied and reapplied, in addition to the Tri-Luma cream, to protect the treated area from sunlight.
Tri-Luma cream - A triple combination specifically designed for melasma treatment. Its active ingredients target:
‒ Hydroquinone - depigmenting agent
‒ Tretinoin - a retinoid that speeds skin cell turnover
‒ Fluocinolone acetonide - a light corticosteroid that reduces inflammation
Mechanism of action of Tri-Luma cream
‒ Hydroquinone - It blocks melanin production by inhibiting tyrosinase, decreasing pigment formation.
‒ Tretinoin - Tretinoin helps skin cell turnover, promoting the shedding of pigmented cells and increasing the penetration of hydroquinone.
‒ Flucinolone acetonide - It reduces inflammation, which helps in stopping melanocytes, thus preventing pigmentation.
This makes Tri-Luma particularly effective compared with single-agent therapy. Tri-Luma is recommended for:
‒ Moderate to severe melasma
‒ People who did not respond adequately to hydroquinone alone
‒ individuals tolerant to combination therapy and under close supervision
Side effects of Tri-Luma cream
Some common side effects of Triluma cream are mild burning, dryness or irritation, skin redness, scaling or peeling, and steroid-related effects if used excessively (e.g., may cause skin thinning with long-term use).
Flucinolone is a corticosteroid, so long-term use is prohibited due to risks of skin atrophy or telangiectasia.
Precautions for Tri-Luma cream
‒ Use strictly as instructed by your dermatologists
‒ Avoid prolonged continuous use
‒ Use along with a sun protection agent
‒ Pregnant and breastfeeding women should avoid the use of the medicine.
‒ avoid using on sensitive areas like the eyes and mouth
Prevention strategies for melasma
Melasma has a high recurrence rate, so long-term prevention is important.
‒ Daily sun protection - Broad-spectrum sunscreen with SPF 30+ (physical blockers like zinc oxide/titanium dioxide often preferred). Reapply sunscreen every 2–3 hours when you are outdoors.
‒ Protection wear - Wear protective clothing. Mindful skincare: avoid irritating products; use gentle, fragrance-free cleansers and moisturisers.
‒ Lifestyle changes - Reduce sun exposure during peak hours.
Melasma is a severe pigmentary disorder influenced by sunlight, hormones, and genetic factors. While it has no impact on physical health, its visible effects can have emotional and psychological consequences. Effective management requires a multifaceted approach involving lifelong sun protection, appropriate use of topical agents (e.g., hydroquinone, tri-luma), adjunctive procedures when needed, and physician supervision to reduce side effects. With consistent care and realistic expectations, many individuals experience meaningful improvement. Consulting a dermatologist is essential for tailored treatment, monitoring, and support.
What is melasma?
Melasma, also known as chloasma or the mask of pregnancy, is a common disorder of hyperpigmentation. It usually appears as a symmetrical brown-grey patch over the cheeks, nose, and upper lip. Rare, but it can also occur on the jawline, forearms, and chest. Pigmentation conditions are usually seen in young adults and middle-aged women. However, the skin issues can also be seen in men.
What causes melasma?
Those who develop melasma have melanocytes (pigment-producing cells) within the affected skin. In women who develop melanoma during pregnancy and who consume oral contraceptive pills on a regular basis, there is a hormonal component involved. Moreover, genetics and exposure to ultraviolet light from the sun also play a crucial role.
How to remove melasma?
Treatment for melasma should aim to reduce hormonal and environmental factors, along with various lightening agents that help fade the hyperpigmentation. Melasma patches are stubborn to treat, but can certainly be improved with good skincare and a follow-up treatment with a dermatologist who is an expert in treating skin issues.
Does melasma resolve with treatment?
Unfortunately, melasma doesn't permanently resolve. Still, dark patches can be significantly improved with consistent treatment, primarily through strict sun-avoidance measures combined with dermatologist-recommended formulations such as hydroquinone, tretinoin, azelaic acid, and chemical peels and lasers for severe cases.
What treatments are best for melasma?
The best treatments for melasma include a combination of prescription topical creams and, sometimes, procedures such as chemical peels, lasers, and microneedling. A dermatologist usually begins treatment with hydroquinone formulations (such as Melalite forte cream) or a triple-combination product, such as Tri-Luma cream. These topical treatments are often paired with a strict sun avoidance program to lighten pigment.
Does a hydroquinone formulation permanently lighten the skin tone?
No, the results are not permanent. Hydroquinone formulations don't cause permanent skin lightening. The effects can be visible within a few months or, at the most, within a few years with regular application as instructed by the dermatologist. If melasma recurs after treatment discontinuation, please talk to your dermatologist regarding the maintenance treatment for melasma.
How to take care of melasma while living with it?
Melasma is a chronic condition with no definitive cure, so it requires a consistent, proactive approach to manage associated symptoms and prevent flare-ups. The key strategy involves gentle skin care, sun protection, and lifestyle modifications (a balanced diet, regular exercise, and drinking enough water to hydrate your skin).
How to apply hydroquinone creams for hyperpigmentation?
You can start applying a thin layer of hydroquinone cream once nightly to the melasma-prone skin, before bedtime. Gently rub the formulation into the skin until it is absorbed. Avoid applying near the corners of the eyes, mouth, nose, or on open wounds.
What is Melalite Forte cream?
Melalite, containing hydroquinone, is used to treat hyperpigmentation. Hydroquinone is a skin lightening agent that reduces the amount of melanin (a skin pigment) that causes the skin to darken.
Is Tri-Luma cream safe to use on facial skin?
For safe use of Tri-Luma cream, be sure to use this cream exactly as prescribed by your dermatologist. One should apply it away from the eyes, nose, and mouth, and avoid open wounds, as these areas are more likely to be irritated. If local irritation becomes severe or persists, discontinue treatment and seek medical help. Moreover, excessive usage may contribute to redness, discomfort, or skin peeling.
What are the benefits of using Tri-Luma cream?
Tri-Luma cream is the most effective treatment for hyperpigmentation, combining the power of three ingredients: Hydroquinone, Tretinoin, and Fluocinolone. It is considered extremely useful in treating melasma, chloasma, freckles, solar lentigines, and post-inflammatory hyperpigmentation. The treatment is more common among people with melasma and post-inflammatory hyperpigmentation.
What are the common side effects of hydroquinone creams?
Common side effects of Hydroquinone creams include irritation, allergic contact dermatitis, inflammation, and stinging. People using hydroquinone forte cream rarely develop ochronosis (a blue-black or grey-blue discolouration).
Does Melalite forte cream contain steroids?
No, Melalite Forte Cream does not contain steroids; it is a pure hydroquinone formulation that works to lighten the skin. It can lighten everything from freckles and acne scars to post-inflammatory marks due to eczema and psoriasis. At the same time, steroids are anti-inflammatory and act on a genetic level.
Can I use moisturiser over Tri-Luma cream?
The triple combination cream is generally applied at bedtime. Yes, you may use moisturiser and other cosmetic products during the day when you are not using this topical medication.
How long does a Hydroquinone formulation take to work?
To see the full effects of a hydroquinone cream, it is essential to use it regularly as instructed by your dermatologist. If you do not see any improvement in your skin's appearance after 2 months of use, consult your dermatologist for further guidance.



20% OFF
On New Registration
Terms and Conditions Apply*
Flat 20% OFF
on your first purchase
20% off only on the product value
Maximum discount value $20
Only one coupon can be used at a time
Coupon code will be mailed on
your registered email address.
Login
Sign up
Flat 20% OFF
on your first purchase
20% off only on the product value
Maximum discount value $20
Only one coupon can be used at a time
Coupon code will be mailed on
your registered email address.
Login
Sign Up
Flat 20% OFF
on your first purchase
20% off only on the product value
Maximum discount value $20
Only one coupon can be used at a time
Coupon code will be mailed on
your registered email address.
Forgot Password ?